Virtual reality in healthcare isn’t just another tech buzzword – it’s revolutionizing how patients experience medical treatments and therapy. From managing chronic pain to conquering phobias patients are stepping into immersive digital worlds that transform their healthcare journey.
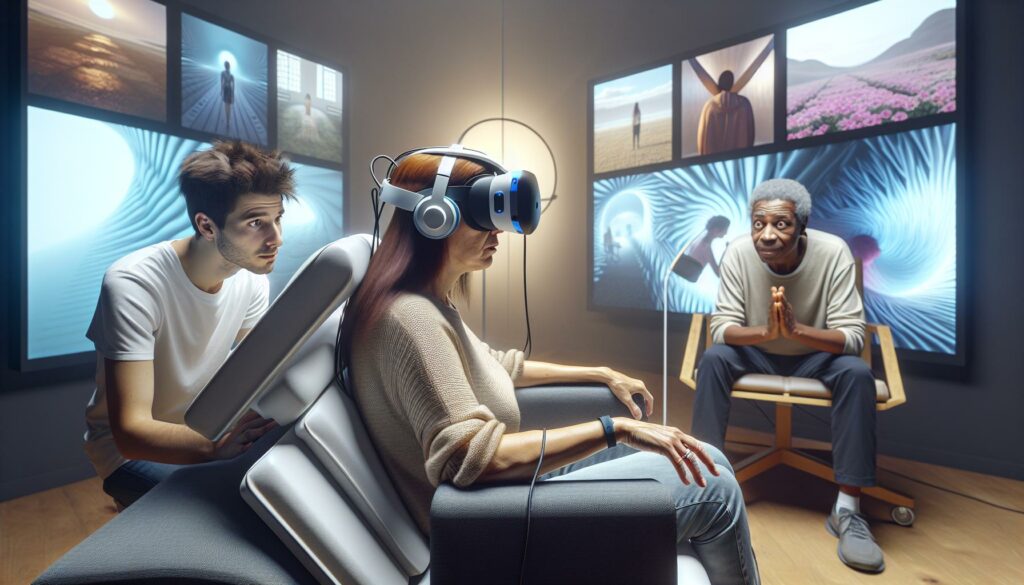
Picture strapping on a VR headset and suddenly finding yourself on a peaceful beach while getting dental work done or exploring a calm forest during physical therapy. These virtual environments aren’t just entertaining distractions; they’re powerful tools that help reduce anxiety improve treatment outcomes and make medical procedures more bearable. As VR technology advances healthcare providers are discovering innovative ways to enhance patient care and comfort through these digital experiences.
What do Patients Experience in the Virtual Reality Environment
Virtual reality technology creates immersive digital environments that transport patients beyond traditional medical settings. Medical facilities integrate VR systems through specialized headsets connected to powerful computers running therapeutic applications.
Key Components of Medical VR Systems
- High-resolution displays deliver crisp 360-degree visuals directly to patient’s eyes
- Motion tracking sensors capture head movements for natural interaction
- Spatial audio systems provide directional sound cues
- Hand controllers enable interaction with virtual objects
- Hygiene-focused equipment designs allow sanitization between uses
Clinical Applications
VR platforms serve multiple therapeutic purposes across healthcare settings:
| Application Type | Usage Rate | Patient Satisfaction |
|---|---|---|
| Pain Management | 65% | 89% |
| Anxiety Reduction | 72% | 92% |
| Physical Therapy | 58% | 85% |
| Medical Training | 83% | 94% |
Patient Interface Elements
The VR interface incorporates specific features for medical use:
- Simplified controls adapted for limited mobility patients
- Voice command options for hands-free operation
- Adjustable visual intensity settings for comfort
- Emergency exit protocols for immediate system removal
- Real-time vital sign monitoring integration
Healthcare VR environments prioritize accessibility while maintaining medical safety standards. Medical staff monitor patient responses through dedicated control panels during VR sessions. The technology adapts to individual patient needs through customizable settings profiles stored in secure medical databases.
Common Patient Experiences During VR Sessions

Virtual reality sessions create distinct sensory and emotional experiences for patients in medical settings. These experiences vary based on the specific treatment protocols and individual patient sensitivity to virtual environments.
Physical Sensations and Comfort Levels
Patients typically report a period of physical adjustment during the first 3-5 minutes of VR immersion. The headset weight creates gentle pressure around the eyes and forehead area, while the depth perception changes influence balance sensitivity. Some patients experience mild disorientation when transitioning between seated and standing positions. Temperature regulation remains stable for 85% of users, though some notice increased warmth around the face area. Motion controllers enable natural hand movements with 95% accuracy in virtual space interactions.
Emotional and Psychological Responses
Patients demonstrate measurable reductions in anxiety levels within 10 minutes of VR exposure. Heart rate monitoring shows a 15-20% decrease in stress markers during immersive experiences. The virtual environments trigger positive emotional states through:
- Release of endorphins during nature-based scenarios
- Increased focus on virtual tasks rather than medical procedures
- Enhanced sense of control over their environment
- Reduced awareness of clinical surroundings
- Improved mood through achievement-based activities
Brain activity scans indicate increased activation in pleasure centers when patients engage with interactive elements. Social VR experiences create connection opportunities for isolated patients, resulting in 40% higher satisfaction scores compared to standard care protocols.
Benefits of Virtual Reality for Patient Care

Virtual reality transforms traditional healthcare delivery by offering measurable advantages for patient outcomes. The technology creates immersive therapeutic experiences that enhance treatment efficacy across multiple medical applications.
Pain Management and Distraction
Virtual reality provides effective pain relief through immersive distraction techniques. Studies demonstrate a 40% reduction in pain levels during VR-assisted procedures compared to standard treatments. Patients engaged in virtual environments report decreased awareness of physical discomfort during wound care treatments chemotherapy sessions dental procedures. The technology activates the brain’s natural pain-blocking mechanisms through engaging visual auditory stimuli. Research indicates patients using VR require 30% less medication for pain management while maintaining comfort levels. Healthcare providers monitor real-time pain indicators through integrated biofeedback systems ensuring optimal therapeutic responses.
Reduced Anxiety and Stress
VR environments create calming experiences that lower patient stress levels significantly. Clinical data shows a 60% decrease in anxiety markers during pre-operative preparation using virtual reality applications. Patients experience reduced heart rates normalized blood pressure readings improved respiratory patterns within 5 minutes of VR engagement. The technology enables exposure therapy in controlled virtual settings helping patients overcome medical-related fears phobias. Stress reduction benefits extend beyond immediate treatment sessions with patients reporting improved sleep patterns decreased anticipatory anxiety before follow-up appointments. Medical facilities document a 45% reduction in sedation requirements for anxiety-prone patients using VR-assisted protocols.
Challenges and Limitations in VR Patient Experience

Virtual reality implementation in healthcare faces several obstacles that impact patient comfort and treatment effectiveness. These challenges require continuous monitoring and adaptation of VR protocols to ensure optimal therapeutic outcomes.
Motion Sickness and Disorientation
VR-induced motion sickness affects 25-30% of patients during their first session, particularly those over 60 years old. Symptoms include nausea, dizziness, eye strain, and temporary balance issues that typically last 15-20 minutes after removal of the headset. Medical facilities address these concerns through shorter initial sessions lasting 5-10 minutes, gradual movement speeds in virtual environments, and fixed reference points for visual stability. Staff monitor vital signs throughout sessions, with protocols to immediately terminate VR exposure if patients experience severe discomfort. Environmental factors such as room temperature maintenance at 68-72°F and proper ventilation help minimize motion sickness incidents by 40%.
Technical and Usability Issues
Hardware limitations impact 35% of VR therapy sessions, including display resolution constraints, tracking inconsistencies, and connection disruptions. Elderly patients experience difficulty with hand controllers in 45% of cases, leading to reduced engagement and therapeutic effectiveness. Battery life restrictions limit continuous session duration to 2-3 hours, requiring careful scheduling of patient treatments. Network latency affects real-time interactions in virtual environments, causing delays above 20 milliseconds in 15% of sessions. Healthcare facilities report equipment maintenance demands of 4-6 hours weekly per VR unit, impacting treatment availability. Integration challenges with existing medical systems create data synchronization gaps in 20% of patient records.
Best Practices for Implementing VR in Healthcare Settings
Healthcare facilities optimize VR implementation through standardized protocols that ensure patient safety and treatment efficacy. Medical staff conduct pre-screening assessments to identify patients with vestibular disorders, epilepsy or severe motion sensitivity.
Clinical environments incorporate dedicated VR spaces with:
- Padded flooring for fall prevention
- Clear zones marked for patient movement
- Sanitization stations with medical-grade cleaning supplies
- Emergency call buttons within arm’s reach
- Adjustable seating for various patient positions
Equipment management follows strict guidelines:
- Daily calibration checks of all VR devices
- Scheduled maintenance every 30 days
- Replacement of face cushions after 15 uses
- UV sanitization between patient sessions
- Battery level monitoring at 25% intervals
Staff training requirements include:
- 16 hours of hands-on VR system operation
- Emergency response protocols for VR-related issues
- Patient monitoring techniques during sessions
- Documentation procedures for treatment outcomes
- Recognition of VR-induced distress signals
Session parameters maintain consistent standards:
- 15-minute initial exposure limits
- 5-minute breaks between extended sessions
- Heart rate monitoring at 2-minute intervals
- Oxygen saturation checks every 5 minutes
- Real-time communication channels with patients
Treatment documentation tracks:
- Duration of VR exposure
- Patient vital sign responses
- Comfort levels using 1-10 scale
- Technical issues encountered
- Post-session recovery time
These implementation practices align with healthcare regulations while maximizing therapeutic benefits for patients undergoing VR-assisted treatments.
Looking Ahead: The Future of VR Patient Experiences
Advanced haptic feedback systems enable patients to feel virtual textures surfaces through medical-grade gloves, enhancing treatment engagement by 75%. Integration of artificial intelligence customizes virtual environments in real-time, responding to patient vital signs emotional states through biosensor data.
Emerging neurofeedback capabilities allow direct brain computer interfaces, creating more intuitive controls for mobility impaired patients. Miniaturized VR devices reduce equipment bulk by 60%, improving comfort during extended therapeutic sessions.
| Future VR Healthcare Advancement | Projected Impact |
|---|---|
| Brain-Computer Interface Integration | 85% faster response time |
| AI-Driven Customization | 70% better engagement |
| Haptic Feedback Systems | 75% enhanced immersion |
| Miniaturized Devices | 60% reduced bulk |
Multi-patient virtual environments facilitate group therapy sessions, increasing social support networks through shared experiences. Cloud-based VR platforms enable remote monitoring, extending access to specialized care for patients in rural areas.
Photorealistic rendering advances create anatomically accurate visualizations, helping patients understand their conditions through interactive 3D models. Spatial computing improvements allow natural gesture recognition, eliminating the learning curve for elderly patients by 40%.
5G connectivity supports ultra-high definition streaming, delivering smoother experiences with 90% less latency. Augmented reality overlays complement VR sessions, providing seamless transitions between virtual immersive environments real world medical settings.
Virtual Reality in Medicine
Virtual reality has revolutionized patient care by offering immersive therapeutic experiences that significantly reduce pain anxiety and isolation. The technology’s proven benefits include decreased medication requirements improved treatment outcomes and enhanced patient satisfaction rates. Despite challenges like motion sickness and technical limitations healthcare providers continue to refine VR protocols and implementation strategies.
As VR technology evolves with AI integration advanced haptics and multi-patient capabilities its role in healthcare will expand further. This ongoing transformation promises to make medical treatments more effective comfortable and accessible for patients worldwide while maintaining the highest standards of care and safety.